From the Encyclopedia of Cleveland
MEDICINE. The development of medical care, science, and education in the Cleveland area, as a frontier community evolved into a major industrial center, is a microcosm of national developments in the U.S. The growth of the population and the financial resources available were determining factors. Although the CONNECTICUT LAND CO. commenced to sell its WESTERN RESERVE lands in 1796, it was not until 1800 that a young Connecticut physician, Moses Thompson (1776-1858), went west, cleared his land, and took up residence in what is today Hudson, OH. For 10 years he was the only physician in the Western Reserve west of Warren, OH. In 1810 DAVID LONG†, from Massachusetts, arrived in Cleveland, 25 miles north of Hudson on Lake Erie, a village of 57 inhabitants. A recent medical graduate, Long came because of the personal solicitation of a local resident who suggested that his income could be supplemented at first by teaching school and selling merchandise, a pattern common to undeveloped areas. Like PETER ALLEN† from Connecticut, who settled in Kinsman, OH, in 1808, Long and Thompson provided civic and cultural leadership in addition to medical care.
The completion of the OHIO AND ERIE CANAL in 1832 made the area more accessible, and by 1837 Cleveland had over 5,000 inhabitants, including 27 medical practitioners. By 1848 the population had doubled to more than 10,000, which quadrupled by 1860, with GERMANS and IRISH immigrants. The medical practitioners reflected the varieties of U.S. medical practice then available: regular physicians (allopaths), homeopaths (see HOMEOPATHY), botanics or Thompsonians, practitioners of electromagnetic medicine and mesmerism, and surgeon dentists (see DENTISTRY). They treated the wide spectrum of human ailments that prevailed in a prescientific medical world, in which the nature of disease was still poorly understood, and in which smallpox was the sole disease for which a preventive procedure, vaccination, was available. As emergencies arose, temporary hospitals (see HOSPITALS & HEALTH PLANNING) were set up, such as the army hospital created in 1813 at FORT HUNTINGTON in Cleveland to care for wounded soldiers of the War of 1812, and the hospital on WHISKEY ISLAND set up for the CHOLERA EPIDEMIC OF 1832. For most mild illness, people treated themselves with home remedies, often obtaining their information from popular medical books. Patent medicines, often very profitable, were widely advertised. Patients went to the doctor’s “shop” only for minor surgery, tooth extraction, and medicines compounded by the practitioner from drugs purchased in Pittsburgh or other larger cities to the east. House calls occupied much of the physician’s day, and often night, until well into the 20th century. Home delivery of infants was nearly universal until the 1920s.
In 1811, to regulate medical and surgical practice in Ohio, the state legislature set up medical districts for the purpose of creating local societies to certify and oversee practitioners. In 1824 the 19TH MEDICAL DISTRICT OF OHIO, comprising Cuyahoga and Medina counties, was designated; David Long was elected the first president. After a succession of name changes, in 1902 the present ACADEMY OF MEDICINE OF CLEVELAND of Cleveland emerged. Late in the 19th century, the state became the licensing agency for Ohio practitioners. The earliest permanent hospitals in the area were created as charitable institutions to care solely for the poor and the homeless. In 1836, when Cleveland, with a population of 4,800, incorporated as a city, the CLEVELAND BOARD OF HEALTH (est. 1832) erected a city infirmary, called City Hospital, the ancestor of Cleveland’s MetroHealth Medical Center.
Medical education quickly followed the population growth. In the early 19th century, most physicians were still educated as house students of practicing physicians; Moses Thompson in Hudson having been such a preceptor. But gradually medical colleges, chiefly proprietary institutions organized locally by enterprising physicians, spread throughout the country. The first in northeast Ohio was established at Willoughby, 15 miles from Cleveland, by a group of physicians who had migrated westward from New York State. Founded in 1834 as the Medical Department of Willoughby Univ. of Lake Erie, the school at first attracted outstanding teachers such as JOHN DELAMATER† (1787-1867) and JARED P. KIRTLAND† (1793-1877), but internal dissension led shortly to their resignation. They created a new school in Cleveland named the Cleveland Medical College. Originally chartered in 1843 as a department of the Western Reserve College of Hudson, this school existed in 1994 as the School of Medicine of CASE WESTERN RESERVE UNIVERSITY
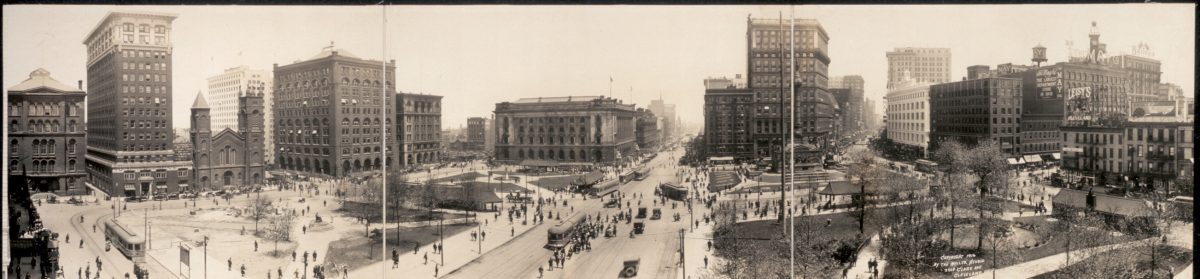
Cleveland also became an educational center for homeopathic physicians, who began to settle in Ohio in the 1830s. In 1846 a homeopathic society was founded and a homeopathic pharmacy opened on PUBLIC SQUARE, and 4 years later the second school of homeopathy in the U.S., the Western College of Homeopathic Medicine, opened. The Cleveland Homeopathic Medical College, as it was later called, remained in existence from 1850 to 1914, when it became a division of Ohio State Univ. in Columbus. Since homeopathy attempted to reform the excesses of “regular” medical practices, opposing massive dosages and polypharmacy and advocating more conservative methods, regular physicians viewed it as heretical. The Cleveland homeopathic community in 1856 opened the first permanent hospital apart from the infirmary in the city. Named the CLEVELAND HOMEOPATHIC HOSPITAL, it treated mainly employees of RAILROADS who were sick or injured away from home. By 1879, since most other area hospitals would not admit homeopathic physicians or surgeons, a large new hospital, the antecedent of HURON RD. HOSPITAL in EAST CLEVELAND (which established the first NURSING training school west of the Alleghenies) was built on Huron Rd. Highly respected by the nonmedical community, a number of homeopathic physicians became community leaders, and at the turn of the 20th century, leading Cleveland citizens such as MARCUS A. HANNA†, MYRON T. HERRICK†, and JOHN D. ROCKEFELLER† supported their institutions.
In the 19th century, modern theories and practices of medicine began to emerge in Western Europe. The microscope revealed microorganisms that Louis Pasteur, Robert Koch, and others demonstrated to be disease-causing agents. It also revealed that the minute structure of the human body is composed of cells. In addition to the 2 new sciences of bacteriology (now microbiology) and cellular pathology, an innovation called anesthesia had been developed by American surgeons, and the English surgeon, Joseph Lister, had developed antiseptic surgical procedures. At the same time, a multitude of new chemical remedies appeared, produced by the new science of organic chemistry. All this new information was rapidly transmitted by European emigres, by an increasing number of medical and surgical periodicals, and by Americans studying abroad.
Because of its strategic location, Cleveland gradually became a rich and growing center of intellectual and cultural resources and attracted talent from both home and abroad. By 1890, with a population of more than 250,000, it had 4 medical schools, 3 medical societies, and 335 physicians, 25% of them homeopaths. The medical community was quick to assimilate new medical knowledge and techniques, and to modify its institutions accordingly. Among the influential figures in Cleveland medical education during this period was GUSTAV C. E. WEBER† (1828-1912), a German-born surgeon who came to Cleveland in 1856, having done postgraduate studies in Vienna, Amsterdam, and Paris. In 1864 he was one of the founders of St. Vincent de Paul Hospital (see SAINT VINCENT CHARITY HOSPITAL AND HEALTH CENTER), where he created a new medical school patterned after Bellevue Medical College in New York City, with student access to clinical as well as didactic teaching. Nearly 20 years later, from 1883-93, after the consolidation of several medical schools, Weber served as dean of the Medical Department of Western Reserve Univ., as the former Cleveland Medical College had been renamed. His successor, Isaac N. Himes (1834-95), who had also studied abroad and who later became Cleveland’s first hospital staff pathologist, raised the Medical Department’s faculty and curriculum to the most advanced standards. A number of its faculty members, such as WILLIAM THOMAS CORLETT†, a dermatologist, John P. Sawyer (d. 1945), a physiologist, and Christian Sihler (1848-1919), a histologist, as well as surgeons FRANK E. BUNTS† (1861-1928) and DUDLEY P. ALLEN† (1852-1915) had also studied abroad. The model for the medical department was the new Johns Hopkins Univ. School of Medicine (est. 1893) in Baltimore, MD. Cleveland search committees turned to Hopkins for new faculty members, such as the pathologist William Travis Howard, Jr. (1867-1953), and the gynecologist HUNTER ROBB†. In 1909, after Abraham Flexner completed his famous survey of American medical schools, he wrote to the president of WRU: “The Medical Department of Western Reserve Univ. is next to Johns Hopkins Univ. . . . the best in the country.”
No advances could have occurred if Cleveland hospitals had not become available for teaching and research. After the Civil War, every decade saw new hospitals established by private charitable corporations (see PHILANTHROPY) or churches (see RELIGION). Some were the progenitors of present-day institutions: the Cleveland City Hospital Assn., organized in 1866, gradually evolved into Lakeside Hospital, modeled on the Johns Hopkins Hospital (1889), and ultimately became a part of UNIVERSITY HOSPITALS CASE MEDICAL CENTER of Cleveland (1931); St. Vincent de Paul Hospital opened in 1865 and continued on its present site; the city infirmary evolved into the Cleveland City Hospital in 1891, which in 1956 became the Cleveland Metropolitan General Hospital, now called MetroHealth Medical Center (see CUYAHOGA COUNTY HOSPITAL SYSTEM (CCHS)). These 3 hospitals and the Huron Rd. Homeopathic Hospital were the first major teaching hospitals in the area. Medical care shifted from the home to the hospital, following the introduction of new diagnostic procedures such as x-ray, bacteriological and chemical laboratories, and aseptic surgical techniques. From the 1880s onward, more hospitals were founded to satisfy various needs, such as maternity, baby, and child care, and for specific populations, such as certain racial groups, women physicians (see WOMAN’S GENERAL HOSPITAL), and residents of SUBURBS. By 1943 there were around 30 hospitals in Cleveland with more than 8,000 beds, not including neighboring communities. The patients were no longer the poor and homeless, but people of every financial status. Physicians made fewer and fewer house calls.
As the causes of epidemic diseases became known, appropriate preventions or treatments were applied. A persistent problem had been typhoid fever–3,460 cases in Cleveland between 1912-26. When William Travis Howard, Jr., brought new pathological and bacteriological methods to Cleveland, he also became the city bacteriologist, a position created especially for him. Both he and his successor, ROGER G. PERKINS† (1912), suspected that the source of the typhoid bacilli was Lake Erie, from which the Cleveland water supply had been pumped since 1856 (see WATER SYSTEM, SANITATION). After extensive research, the problem was finally corrected by Oct. 1925, with complete filtration and chlorination of the lake water. Infant mortality had also been very high, with deaths caused by diarrhea, dehydration, and malnutrition, especially among the offspring of immigrants from Southern and Eastern Europe (see IMMIGRATION AND MIGRATION). The Milk Fund Assn., founded in 1899 as a private charitable organization, and the Babies’ Dispensary & Hospital, incorporated in 1904 under the aegis of Edward Fitch Cushing (1862-1911) and HENRY JOHN GERSTENBERGER†, provided care for poor children and freed them from milkborne pathogens. In 1912 the city Health Department established a Bureau of Child Hygiene, which set up 12 dispensaries throughout the city and oversaw the milk production and distribution from its own dairy farm, aided by volunteers. Also, the VISITING NURSE ASSN. OF CLEVELAND brought medical supervision and care into the homes of the poor (see PUBLIC HEALTH). Pediatrics began to develop as a strong medical specialty. Gerstenberger, with postgraduate training in Berlin and Vienna, was appointed professor of pediatrics at the WRU School of Medicine in 1913, when the first separate department was established. He collaborated with a research chemist in developing SMA, a best-selling synthetic milk for infants, the income from which helped to create what became Rainbow Babies & Childrens Hospital (opened in 1925) of Univ. Hospitals. Cleveland became a major center for the training of pediatricians.
During World War I, GEORGE W. CRILE† organized a group of Lakeside Hospital physicians, surgeons, nurses, and enlisted men to serve in France (seeLAKESIDE UNIT, WORLD WAR I). (After WORLD WAR II broke out, on Christmas Eve 1941, the U.S. surgeon general invited the unit to be first again. A month later, the Clevelanders organized as the FOURTH GENERAL HOSPITAL.) While working together in France, surgeons Crile, his cousinWILLIAM E. LOWER†, and Frank E. Bunts recognized the advantages of group clinical practice; after returning, they invited internist JOHN PHILLIPS† to join them and established the CLEVELAND CLINIC FOUNDATION (1921). Crile had already distinguished himself nationally, by performing the first successful human blood transfusion in 1906, by his research on shock, and by his reputation for thyroid surgery. The Cleveland Clinic rapidly acquired a national and international reputation for specialization and quality care. Gases produced in a fire in 1929 (see CLEVELAND CLINIC DISASTER) caused many deaths, including that of founder John Phillips. The fire ultimately saved other lives worldwide, however, since it led to the development and use of nontoxic x-ray film.
After World War I, an affluent and growing Cleveland arranged to have a survey made of its hospitals to improve the quality of health care. The 1,082-page Cleveland Hospital & Health Survey (1920), one of the first in an American city, was carried out by an outside expert, Haven Emerson. Cleveland has pioneered in many other forms of cooperation and teamwork, such as the CLEVELAND HOSPITAL SERVICE ASSN. (est. 1934, later renamed BLUE CROSS OF NORTHEAST OHIO) and the Community Health Foundation (est. 1964), the first health-maintenance organization in the Middle West, nowKAISER PERMANENTE MEDICAL CARE PROGRAM. In addition, the Cleveland Health Education Museum (later the HEALTH MUSEUM), the first in the U.S., opened in 1940.
In the 1930s, innovators such as JOSEPH T. WEARN† at the WRU School of Medicine and Russell L. Haden at the Cleveland Clinic brought laboratory-oriented medical science to the forefront. Obstetricians from Cleveland hospitals, led by A. J. SKEEL† of SAINT LUKE’S MEDICAL CENTER, in 1932 formed the Cleveland Hospital Obstetric Society, which for 10 years collected data and analyzed the causes of maternal mortality, stimulating similar activity in other cities and influencing standards of the American College of Surgeons. Many cooperative medical events have occurred, such as the 1962 polio immunization campaign sponsored by the Cleveland Academy of Medicine and the Cuyahoga County Medical Foundation. On Sabin Oral Sundays, 2,400 physicians and other volunteers distributed sugar cubes containing polio vaccine and immunized more than 84% of the Cuyahoga County residents, the best record in the U.S. This success was facilitated by voluntary action, advertising, and public-relations expertise from the nonmedical community (seePHILANTHROPY). Earlier, in 1949, Cleveland radiologists had cooperated with the Academy of Medicine, the Antituberculosis Society, and the Greater Cleveland Hospital Assn. in a successful mass survey to detect tuberculosis among Greater Cleveland citizens.
One may finally ask, what are some of the unique contributions of Cleveland medicine? What, if any, major medical discoveries have been made? Medical “firsts” include Noah Worcester’s first American treatise on dermatology, A Synopsis of the Symptoms, Diagnosis, and Treatment of the More Common and Important Diseases of the Skin (Philadelphia, 1845); Abraham Metz’s first textbook on ophthalmology, The Anatomy and Histology of the Human Eye(Philadelphia, 1869); and Samuel W. Kelley’s first book on pediatric surgery, The Surgical Diseases of Children: A Modern Treatise on Pediatric Surgery(New York, 1909). On 8 Feb. 1896, 3 months to the day after Wilhelm Konrad Roentgen in Germany announced the discovery of x-rays, DAYTON C. MILLER†, a professor at Cleveland’s Case School of Applied Science, made the first x-rays in the U.S. He lectured 2 months later to the CLEVELAND MEDICAL SOCIETY. There were outstanding teachers, such as William Thomas Corlett, appointed in 1901 as one of the few American physicians to test the new syphilis remedy, Salvarsan, at Lakeside Hospital, CARL J. WIGGERS† (called the father of hemodynamics in the U.S.), the first editor ofCirculation Research, and TORALD H. SOLLMANN†, who in 1901 published the leading American textbook on pharmacology, which has gone through at least 8 editions. Endemic goiter has disappeared because of the research between 1915-20 of DAVID MARINE† and CARL H. LENHART† that showed that it was caused by iodine deficiency in the diet.
Since 1940 Cleveland’s major medical contributions have been in cardiovascular diseases and their treatment: the studies of angina pectoris carried out by Harold Feil and Mortimer Siegel at MT. SINAI MEDICAL CENTER and their pioneering work in electrocardiography; the experiments of HARRY GOLDBLATT† in hypertension; and the development of open-heart surgery by CLAUDE S. BECK† (who also gave the first course in cardiopulmonary resuscitation, later called CPR, 1950), and Jay Ankeney at Univ. Hospitals. In 1956 St. Vincent Charity Hospital opened the world’s first intensive-care unit devoted exclusively to heart surgery. Willem Kolff developed kidney dialysis techniques at the Cleveland Clinic, where he also started to develop the artificial heart, aided by research engineers at the NASA JOHN H. GLENN RESEARCH CENTER AT LEWIS FIELD. Cleveland Clinic became a “revascularization center” for coronary artery disease by means of bypass surgery, based on a technique developed by Ten Nobel laureates have been affiliated with the CWRU medical school, including Frederick C. Robbins, honored for his work with the polio virus. Other Cleveland contributions to medicine included pioneering work in gerontology, the activities of the CLEVELAND MEDICAL LIBRARY ASSN. (est. 1894), and the first and longest-running medical feature on a television news show, Dr. Theodore Castele’s segment of “Live on 5” (WEWS (Channel 5)), which began in 1975. In 1990 national attention focused on Univ. Hospitals researchers, headed by Dr. Roland W. Moskowitz, who traced osteoarthritis to a specific genetic defect; in 1993 Dr. Eric Topol concluded a 2-year study, the largest of its type, on the effects of the drug t-PA on heart attack patients. One can characterize medicine in Cleveland as equal and in many cases superior to that of other urban centers. In the 20th century, it has been especially distinguished by extensive institutional cooperation and outstanding private and community support.
Genevieve Miller
Case Western Reserve Univ. (emeritus)
Brown, Kent L., ed. Medicine in Cleveland and Cuyahoga County: 1810-1976 (1977).
Dittrick, Howard, comp. Pioneer Medicine in the Western Reserve (1932).
Waite, Frederick Clayton. Western Reserve University, Centennial History of the School of Medicine (1946).